Artificial Platelets: A Lifesaving Breakthrough for Trauma Victims
Researchers have created artificial platelets, which provide a novel way to buy trauma victims vital time during emergencies. With its ability to respond quickly to severe bleeding, this advancement in artificial organs has the potential to completely transform emergency medical care.
Artificial Platelets: A Revolutionary Step in Trauma Care
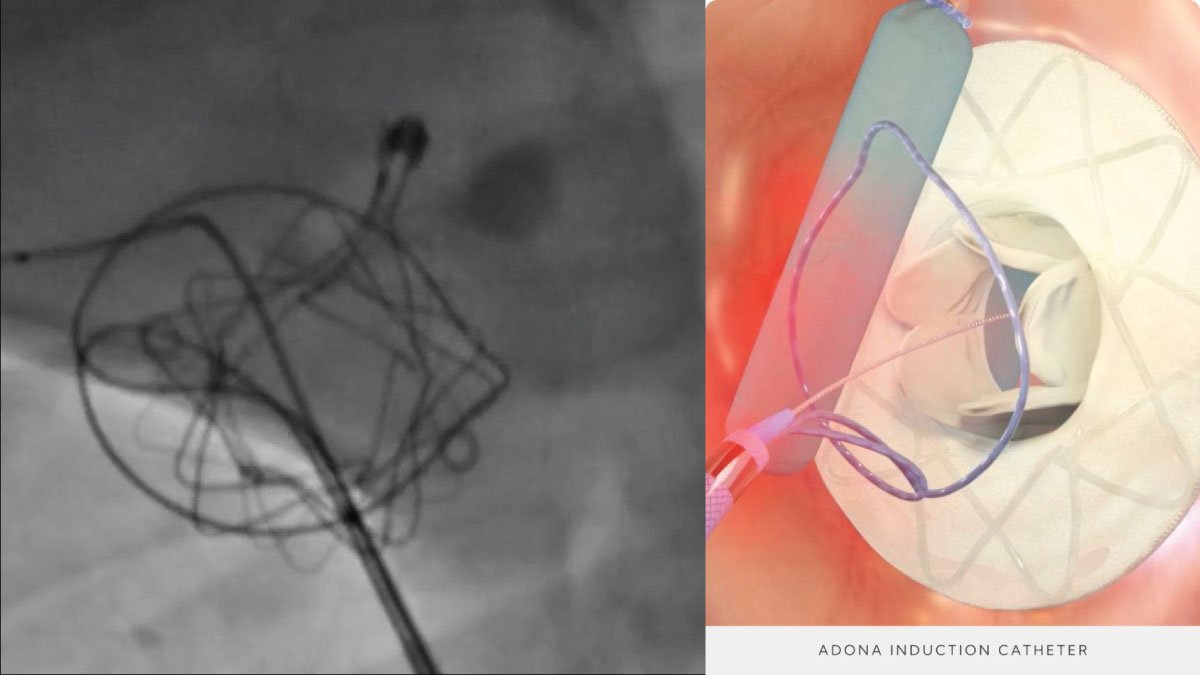
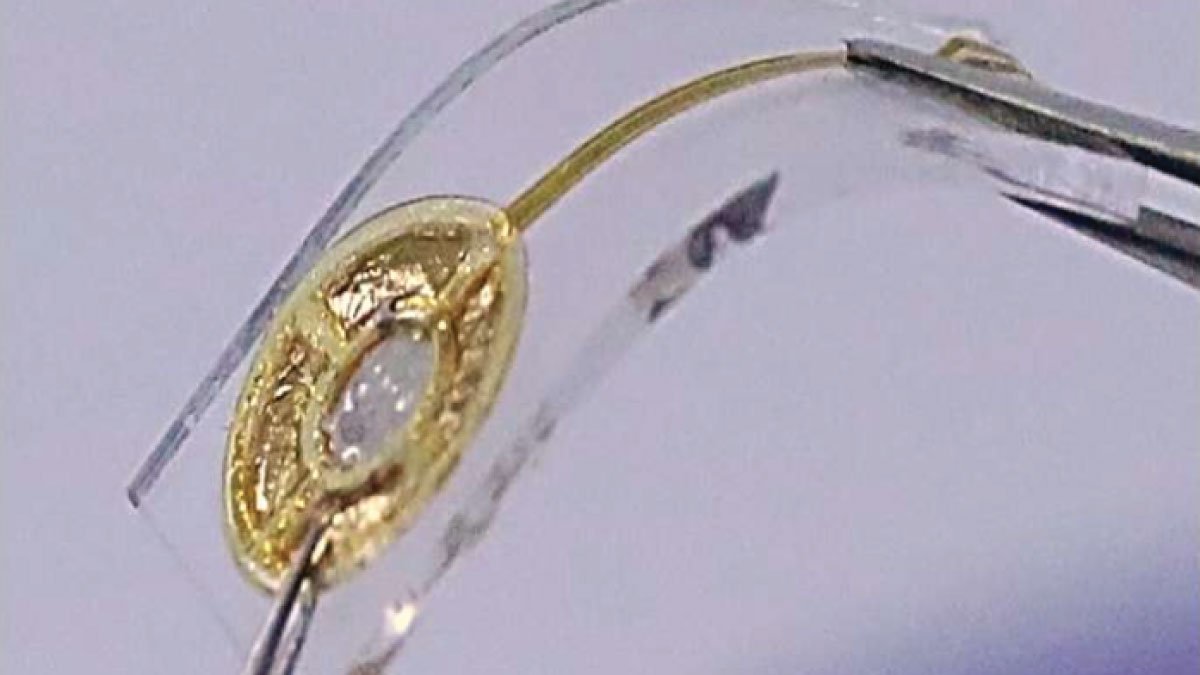
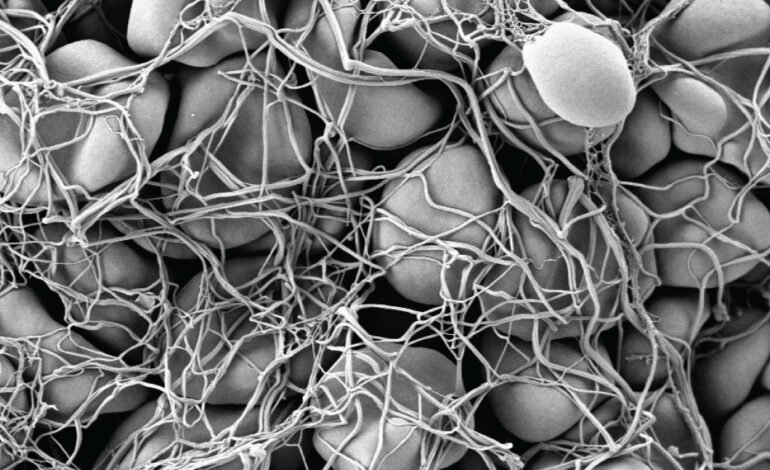
Researchers at Chapman University and other top universities have made artificial platelets, a ground-breaking discovery that can greatly enhance the treatment of severe bleeding in trauma victims. Because it offers instant hemostasis, this cutting-edge device has the potential to revolutionize trauma care by essentially buying patients in critical conditions some extra time. These platelets, in contrast to conventional therapies, act by imitating natural platelets, quickly forming clots and stopping blood loss. In emergency medicine, where every second counts, this innovation is critical.
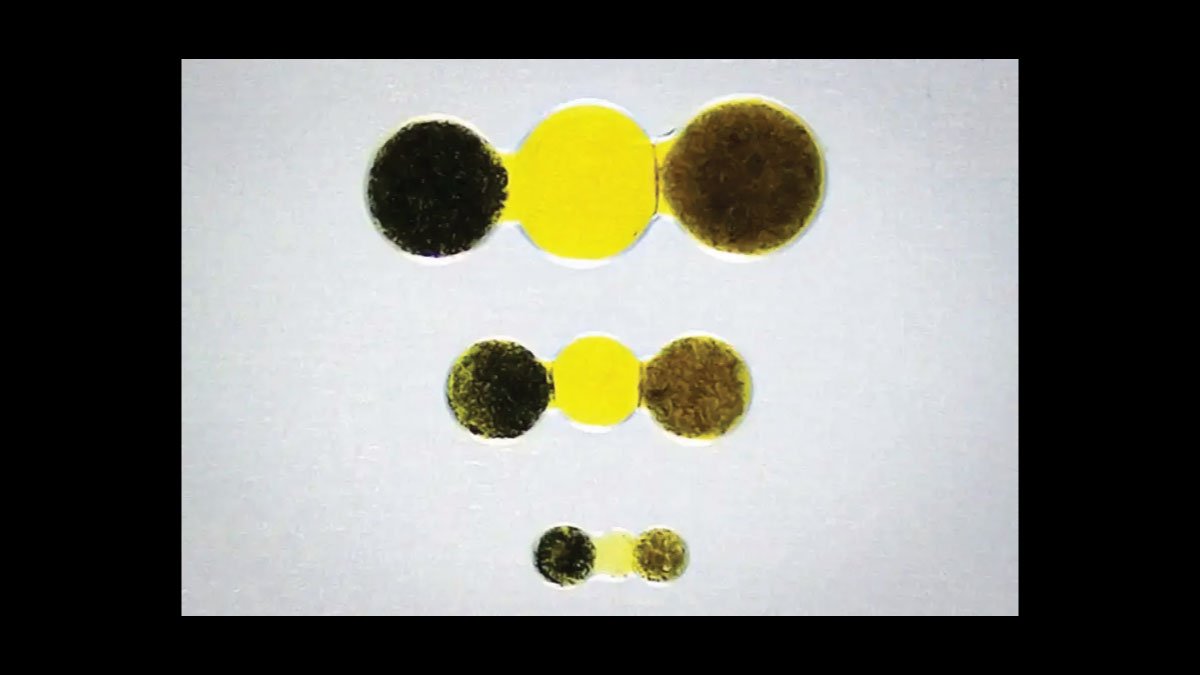
These artificial platelets were created by a group of researchers under the direction of Dr. Ashley Brown in order to overcome the drawbacks of current hemostatic drugs and blood transfusions. Dr. Brown claims that compared to conventional therapies, the artificial platelets have demonstrated amazing performance in preclinical experiments, cutting bleeding time by up to 50%. When it comes to saving lives in an emergency, this notable improvement in response time could literally change the game.
Benefits and Uses of Artificial Platelets
- Quick Reaction: In the event of serious bleeding, artificial platelets can be quickly distributed at the site of injury, guaranteeing a prompt intervention. This ability is especially important when there is no immediate access to medical care.
- Decreased Blood Loss: They can quickly form clots by imitating the activity of real platelets, which minimizes blood loss and lowers the chance of subsequent issues. This is an important part of keeping the patient stable and avoiding shock.
- Stability and Compatibility: There is no requirement for blood type matching because the artificial platelets are made to be compatible with all blood types. Moreover, they exhibit stability at room temperature, rendering them convenient to handle and move, especially in isolated or resource-constrained environments.
- Non-Invasive and Safe: The platelets can be injected intravenously, reducing patient discomfort and infection risk, in contrast to certain current treatments that call for invasive procedures.
Future Trends and Potential Applications
Artificial platelets have shown promise in preclinical experiments, opening the door to possible applications in a range of medical settings. Their use in surgical operations, when there is a high danger of severe bleeding, is being investigated by researchers. Combining artificial platelets with other biomedical engineering advancements, including intelligent drug delivery systems, may increase their efficacy and expand their range of uses. Innovations like these are expected to be vital in enhancing patient outcomes and revolutionizing trauma care as the area of artificial organs continues to develop.
Conclusion
The creation of artificial platelets represents an important advancement in emergency care by providing a vital tool for treating severe bleeding in trauma patients. The breakthrough offer a prompt and efficient reaction to life-threatening circumstances where every second counts, thanks to their rapid mimicking of the clotting action of natural platelets. With more investigation and a closer approach to clinical application, these artificial platelets have the potential to revolutionize trauma care, increase survival rates, and even save countless lives. These are at the front of an exciting new development that could revolutionize the field of trauma care.