Personalized Stem Cell Islet Tissue Offers New Hope for Type 2 Diabetes Treatment

A revolutionary research study highlights the potential of custom-made endoderm stem cell-grown islet tissue in treating individuals with impaired function of pancreatic islets, marking a significant breakthrough in the field of personalized medicine for type 2 diabetes.
Cutting-Edge Personalised Stem Cell Islet Tissue Therapy for Type 2 Diabetes
Latest developments in the field of personalized medicine have paved the way for a groundbreaking therapy for type 2 diabetes (T2D) that uses endoderm stem cell-grown islet tissue. This cutting-edge method presents a hopeful solution for those with impaired pancreatic islet function, a critical factor in the onset and progression of type 2 diabetes.
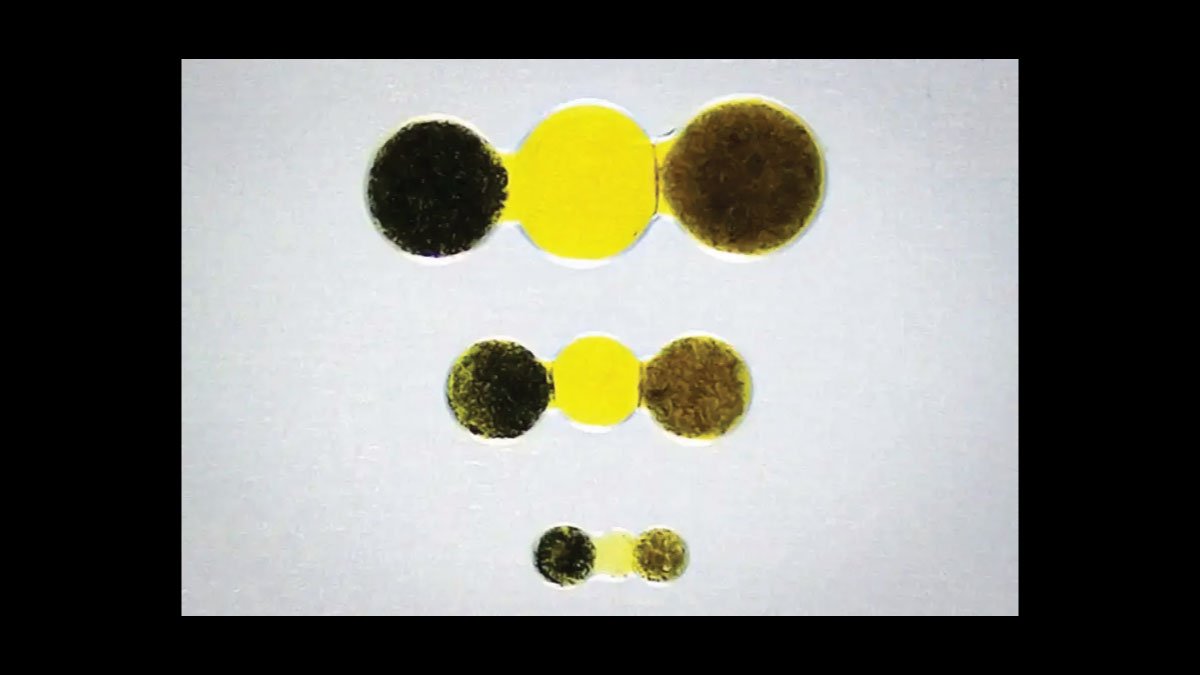
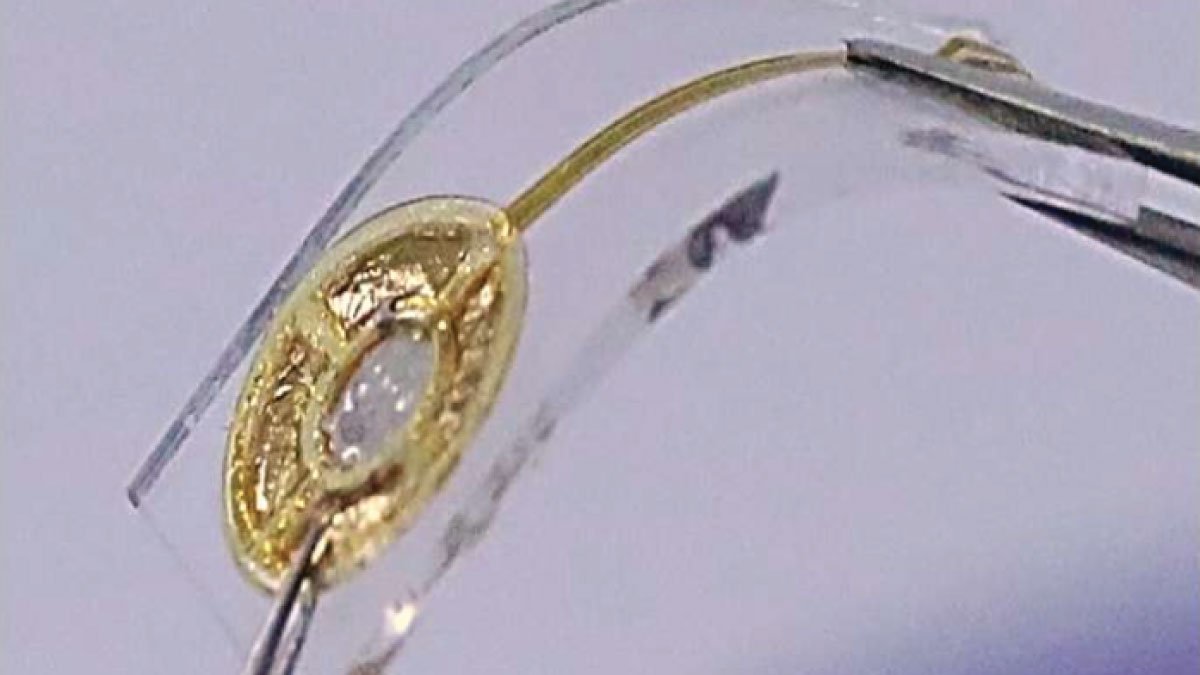
The research, featured in Translational Medicine, details the success of employing personalized stem cell therapy to produce functional pancreatic islet cells. These cells are created from endoderm stem cells, which are engineered to become insulin-producing islet cells. This technique has demonstrated significant promise in restoring the regulation of blood sugar in individuals whose pancreatic islets are not functioning properly.
Benefits of Personalized Stem Cell Islet Tissue
- Individualized Treatment: This technology differs from conventional therapies by allowing the creation of islet tissue specifically designed for each patient’s genetic and biological characteristics. This customization increases the chances of a successful treatment outcome.
- Recovery of Pancreatic Function: By implanting personalized islet tissue, this treatment tackles the fundamental issue of diabetes—the malfunctioning of pancreatic islets. This can lead to enhanced control of blood sugar levels and a reduced reliance on insulin injections or oral medications.
- Lower Risk of Side Effects: Custom-made islet tissue may reduce the risk of side effects common with traditional diabetes treatments, such as insulin resistance and hypoglycemia, by offering a more natural and effective solution for managing glucose levels.
- Sustained Effectiveness: Preliminary findings suggest that this method may provide lasting benefits by potentially reversing the damage to pancreatic islets and improving metabolic control over time.
Conclusion
The application of personalized stem cell islet tissue marks a significant breakthrough in the treatment of type 2 diabetes. By customizing therapies to fit each patient and addressing the root cause of diabetes—the dysfunction of pancreatic islets—this technology brings new hope for better management and potential remission of the disease. As research continues, this innovative approach is set to transform diabetes care and establish new benchmarks in personalized medicine.